COVID-19 and Hypertension: Exploring the Links and Risks

In the midst of the ongoing global impact of COVID-19, an illness caused by the novel coronavirus SARS-CoV-2, specific patient demographics and pre-existing health conditions have emerged as crucial determinants of disease severity and outcomes. Among these conditions, hypertension, commonly known as high blood pressure, has been consistently observed in severe cases of COVID-19.
Exploring the Connection: COVID-19 and Hypertension
The correlation between COVID-19 and hypertension has become a subject of extensive investigation and scholarly research. Unraveling the precise link necessitates a thorough examination of various mechanisms that contribute to this association. These mechanisms include the upregulation of angiotensin-converting enzyme 2 (ACE2), the presence of co-existing comorbidities, and the potential impact on the immune response.
Factors Description Angiotensin-converting enzyme 2 (ACE2) Upregulation Individuals with hypertension frequently demonstrate heightened levels of ACE2 receptors. These receptors act as gateways for the SARS-CoV-2 virus, facilitating its invasion of host cells and initiating infection. The escalated expression of ACE2 receptors among hypertensive patients implies that they might be more susceptible to viral entry and subsequent propagation. Co-existing Comorbidities Hypertension often occurs alongside other chronic conditions like diabetes, cardiovascular diseases, and kidney diseases. These comorbidities commonly accompany hypertension and can additionally impair the immune response. Individuals with hypertension and these co-existing conditions may experience compromised immune systems, rendering them more susceptible to severe infections, including COVID-19. Immunological Response Hypertension possesses the capacity to influence immune responses within the body. It is hypothesized that hypertension can induce immune dysfunction, compromising the body’s ability to mount an effective defense against infections. This compromised immune response could potentially contribute to the heightened severity of COVID-19 among individuals with hypertension.
It is crucial to acknowledge that research in this area is still in progress, and our comprehension of the connection between COVID-19 and hypertension is continually advancing. Further investigations are necessary to comprehensively unravel the underlying mechanisms and devise effective strategies for managing COVID-19 in individuals with hypertension.
The ACE2 Connection
ACE2 is a protein that resides on the surface of various cell types and plays a role in regulating blood pressure and heart function. It serves as a crucial point of interaction for SARS-CoV-2, enabling the virus to enter human cells and replicate.
Interestingly, ACE2 is also a vital component of the renin-angiotensin-aldosterone system (RAAS), which is a hormonal cascade essential for blood pressure regulation. Certain medications used to treat high blood pressure, such as ACE inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), function by modulating this system.
Initially, concerns arose regarding whether these medications might increase ACE2 levels and, consequently, raise the susceptibility to or severity of COVID-19. However, a substantial body of evidence, including a report from the New England Journal of Medicine, indicates that these medications do not elevate the risk or severity of COVID-19. Major health organizations, including the World Health Organization (WHO), American Heart Association (AHA), and European Society of Cardiology (ESC), concur that individuals should continue taking these medications as prescribed.
Comorbidity Complications
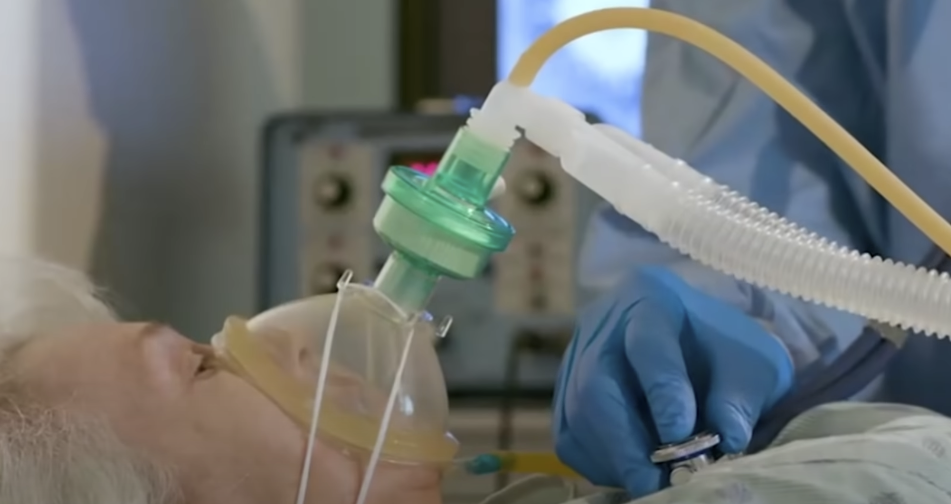
Hypertension seldom exists as a solitary health concern. It frequently accompanies other medical conditions, substantially amplifying the likelihood of severe disease outcomes when individuals with hypertension contract COVID-19.
The table below provides a summary of the impact of common comorbidities on the severity of COVID-19 in hypertensive patients:
Comorbidity Influence on COVID-19 Severity Cardiovascular Diseases The presence of hypertension adds strain to the heart, consequently elevating the risk of severe disease outcomes. Diabetes Hypertension alters the immune response, thereby increasing the risk of complications related to COVID-19. Obesity Hypertension contributes to respiratory dysfunction and can result in worse disease outcomes. Kidney Diseases Hypertension increases the risk of acute kidney injury during COVID-19 infection.
Immunological Alterations
Chronic hypertension has the potential to trigger immune dysregulation, resulting in a compromised immune response. It is speculated that this immune dysfunction may facilitate more efficient viral replication in the early stages of the disease, thereby contributing to more severe disease outcomes.
Hypertension Management Amid COVID-19
Given the implications of hypertension on COVID-19 severity, effective hypertension management becomes even more critical during the pandemic. Here are several measures to mitigate risks:
- Maintain Regular Medication: Discontinuation of antihypertensive medication can lead to uncontrolled blood pressure and associated complications. Patients should continue their prescribed medication unless advised otherwise by their healthcare provider;
- Monitor Blood Pressure at Home: Regular monitoring can detect any anomalies early, facilitating timely medical intervention;
- Lifestyle Modifications: Regular physical activity, a balanced diet, limited alcohol consumption, and smoking cessation are key to managing hypertension effectively;
- Follow COVID-19 Guidelines: Observing safety measures such as wearing masks, social distancing, regular hand hygiene, and COVID-19 vaccination is paramount.
Conclusion
The COVID-19 pandemic has underscored the need for comprehensive understanding and effective management of hypertension. As we continue to combat this health crisis, it’s paramount to keep the conversation focused on the risks and implications of such comorbid conditions. Efforts must be streamlined towards managing these chronic conditions to mitigate their impact on COVID-19 outcomes
FAQS
Current research indicates that blood pressure medications, such as ACE inhibitors and ARBs, do not increase the risk of contracting or exacerbating COVID-19.
Yes, as hypertension has been linked to severe COVID-19 outcomes, it is prudent to follow all COVID-19 preventative measures diligently.
No, do not discontinue your medication unless specifically instructed by your healthcare provider.
No, the risk can vary depending on age, the presence of other comorbidities, and overall health status.