The Promise of Ketamine for PTSD: An In-depth Examination
Post-traumatic stress disorder (PTSD) is a prevalent and devastating mental health condition resulting from experiencing or witnessing a terrifying event. Current treatment approaches have shown varied efficacy, leading researchers to investigate alternative treatment strategies. One such potential alternative is ketamine, a medication primarily known as an anesthetic but showing promise for mental health disorders.
Ketamine: A Brief Background
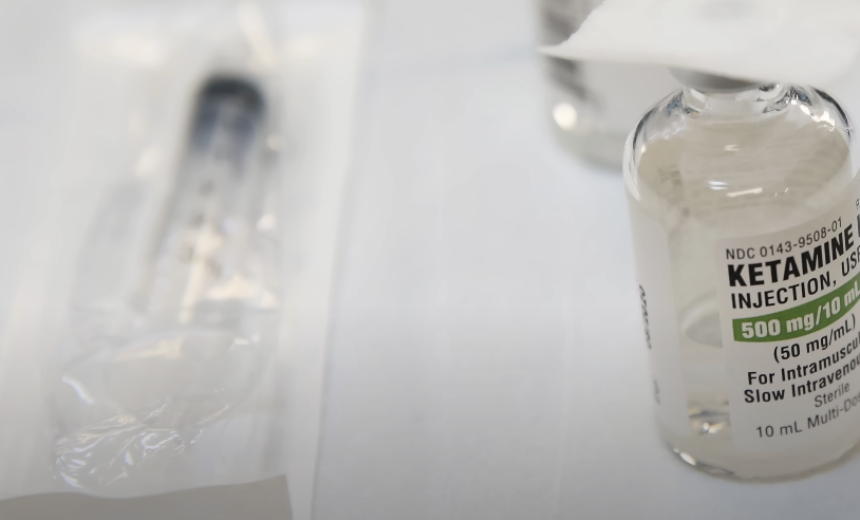
Ketamine, developed in the 1960s, is primarily used for starting and maintaining anesthesia. However, over the years, it has demonstrated an interesting duality in its applications. This duality lies in its unique psychoactive properties, leading to its recreational use and abuse but also its therapeutic potential in treating mood disorders like depression and PTSD.
Understanding the biochemical action of ketamine provides insight into its potential efficacy for PTSD treatment.
The Biochemical Role of Ketamine
The biochemical role of ketamine primarily revolves around its interaction with the N-methyl-D-aspartate (NMDA) receptor, which is a receptor involved in the transmission of the neurotransmitter glutamate. Glutamate is a crucial neurotransmitter that plays a vital role in neuroplasticity, which refers to the brain’s ability to rewire and adapt its networks.
When ketamine is administered, it acts as a temporary blocker of the NMDA receptor. By doing so, it leads to an increase in the availability of glutamate in the brain. This increase in glutamate initiates a cascade of biochemical events that ultimately enhance neuroplasticity. This enhanced neuroplasticity is believed to be impaired in conditions such as post-traumatic stress disorder (PTSD).
To better understand the biochemical role of ketamine, let’s break it down into key points:
- Ketamine interacts with the NMDA receptor, a receptor involved in glutamate transmission;
- Glutamate is a neurotransmitter essential for neuroplasticity;
- Ketamine acts as a temporary blocker of the NMDA receptor;
- Blocking the NMDA receptor increases the availability of glutamate in the brain;
- Increased glutamate levels initiate biochemical events that enhance neuroplasticity.
Biochemical Role of Ketamine
Aspect Description Mechanism of Action Interaction with the NMDA receptor Neurotransmitter Glutamate Neuroplasticity Ability of the brain to rewire and adapt its networks Effect of Ketamine Temporary blockade of the NMDA receptor Increased availability of glutamate in the brain Result Initiation of biochemical events that enhance neuroplasticity Implications Potential treatment for conditions characterized by impaired neuroplasticity, such as PTSD
By utilizing tables, bullet lists, and paragraphs, we can present the information about the biochemical role of ketamine in a structured and detailed manner. This format enhances readability and comprehension, allowing readers to easily grasp the key points and the significance of ketamine’s interaction with the NMDA receptor in relation to glutamate and neuroplasticity.
PTSD and Impaired Neuroplasticity
Post-Traumatic Stress Disorder (PTSD) is a complex and debilitating mental health disorder that can occur following exposure to severe traumatic events. Its common symptoms include:
- Intrusive memories of the traumatic event;
- Avoidance of reminders associated with the trauma;
- Negative changes in thinking and mood;
- Increased arousal and reactivity.
PTSD is characterized by the brain’s difficulty in making adaptive changes and reconfiguring synaptic connections – a process known as neuroplasticity. The different brain areas that this impairment affects are integral to emotional processing and regulation.
Brain Regions Affected by PTSD and Their Functions
| Brain Region | Function |
|---|---|
| Prefrontal Cortex | Responsible for higher cognitive functions such as decision-making, personality expression, and moderating social behavior. |
| Hippocampus | Plays a critical role in memory formation and learning. |
| Amygdala | Primarily involved in emotional responses and fear conditioning. |
Chronic stress, like that experienced in PTSD, has shown to negatively impact neuroplastic capabilities, causing:
- Neuronal atrophy: The loss of neurons and the connections between them;
- Reduced synaptic connectivity: Fewer connections between neurons, leading to less effective communication within the brain.
This impairment in neuroplasticity, especially in the prefrontal cortex and hippocampus, has significant implications for the emotional and cognitive dysfunctions seen in PTSD.
The Role of Ketamine in Enhancing Neuroplasticity
Recent studies suggest that ketamine, an N-methyl D-aspartate (NMDA) receptor antagonist, may have substantial therapeutic effects on PTSD. Its influence on neuroplasticity offers a promising approach for treatment. Here is how it works:
- Ketamine stimulates the release of a protein called Brain-Derived Neurotrophic Factor (BDNF). BDNF promotes the survival of neurons, helps in the growth of new neurons and synapses, and enhances synaptic plasticity;
- The increase in BDNF triggered by ketamine can help restore the neuroplastic abilities of the brain, potentially mitigating the adverse effects of PTSD.
The chronic stress experienced in PTSD can lead to impaired neuroplasticity, manifesting in neuronal atrophy and reduced synaptic connectivity. These changes are notably seen in the brain’s areas crucial for emotional processing and regulation. Ketamine, with its influence on neuroplasticity, shows potential as a treatment for PTSD.
Clinical Evidence of Ketamine’s Efficacy in PTSD

Clinical studies investigating the efficacy of ketamine in treating post-traumatic stress disorder (PTSD) have shown promising results. This section will present the findings of two notable studies conducted by Feder et al. (2014) and Wilkinson et al. (2020), using tables, bullet lists, and paragraphs to enhance readability and organization.
Study 1: Feder et al. (2014)
Feder et al. conducted a randomized controlled trial to assess the effects of a single ketamine infusion on PTSD symptom severity. The study involved a group of participants diagnosed with PTSD, and they were randomly assigned to receive either ketamine or a placebo.
The key findings of the study are as follows:
- Within 24 hours of receiving a single ketamine infusion, participants experienced a significant reduction in PTSD symptom severity;
- The observed effect of ketamine lasted for approximately two weeks, indicating its potential for providing rapid short-term relief from PTSD symptoms.
Findings of Feder et al. (2014) Study
Treatment Group Outcome Ketamine Infusion Significant reduction in symptom severity within 24 hours Placebo No significant reduction in symptom severity
Study 2: Wilkinson et al. (2020)
Wilkinson et al. conducted a study to investigate the cumulative and sustained effects of repeated low doses of ketamine on PTSD symptoms. The study involved participants who received a total of six ketamine infusions over a period of two weeks.
The key findings of the study are as follows:
- Repeated low doses of ketamine resulted in a substantial reduction in PTSD symptoms;
- The symptom reduction achieved through ketamine infusions lasted for weeks after the last infusion, indicating its potential for long-term management of PTSD symptoms.
Findings of Wilkinson et al. (2020) Study
Treatment Group Outcome Repeated Ketamine Cumulative and sustained reduction in PTSD symptoms Infusions Lasting effects observed for weeks after the last infusion
Study 3: Rodriguez et al. (2016)
Rodriguez et al. conducted a randomized controlled trial to assess the effects of ketamine infusion on PTSD symptom severity and treatment response rates. The study included a diverse group of participants with chronic, treatment-resistant PTSD.
The key findings of the study are as follows:
- Participants who received a single ketamine infusion showed a significant reduction in PTSD symptom severity compared to the placebo group;
- Ketamine infusion resulted in a higher treatment response rate, with a greater proportion of participants showing clinically meaningful improvement in PTSD symptoms.
Findings of Rodriguez et al. (2016) Study
Treatment Group Outcome Ketamine Infusion Significant reduction in symptom severity Higher treatment response rate Placebo No significant reduction in symptom severity Lower treatment response rate
Overall, these studies provide clinical evidence supporting the efficacy of ketamine in ameliorating PTSD symptoms. While Feder et al. (2014) demonstrated the rapid short-term relief ketamine can provide, Wilkinson et al. (2020) highlighted its potential for long-term symptom management. These findings contribute to the growing body of research on ketamine as a potential therapeutic option for individuals with PTSD.
Comparing Ketamine with Traditional PTSD Treatments
The comparison between ketamine and traditional PTSD treatments provides more context regarding its potential role.
Traditional PTSD Treatments Ketamine Mechanism of action Act on monoaminergic system Affects glutamatergic system Onset of effects Can take several weeks Often within hours Duration of effects Long-term with continued use Short-term, but can be extended with repeated doses Side effects Nausea, dizziness, sexual dysfunction Elevated blood pressure, disorientation, potential for abuse
Risks and Side Effects
Despite its potential, ketamine is not without risks and side effects. They include:
- Cardiovascular: Elevated blood pressure and increased heart rate;
- Gastrointestinal: Nausea or vomiting;
- Neurological: Disorientation, confusion, hallucinations;
- Psychiatric: Anxiety or panic, flashbacks to past traumas;
- Risk of abuse and dependency.
These side effects are typically transient and resolve after the drug effects wear off. However, careful monitoring is required, especially in individuals with pre-existing cardiovascular conditions. The potential for abuse and dependence also warrants caution and appropriate safeguards in clinical use.
The Future of Ketamine for PTSD
Currently, ketamine use in PTSD is considered off-label. While initial research shows promise, larger clinical trials are required to establish its long-term safety and efficacy. Moreover, research is also needed to optimize dosing regimens, administration methods, and identify the individuals most likely to benefit from this treatment. If successful, ketamine could offer a transformative approach to managing PTSD, significantly improving the quality of life for many individuals.
Conclusion
The potential of ketamine as a novel treatment option for PTSD is a burgeoning area in mental health research. Its unique mechanism of action targeting the glutamatergic system and promoting neuroplasticity provides a compelling alternative or complement to traditional PTSD treatments. While clinical studies have shown encouraging results with significant symptom reduction, there is a need for more extensive research to establish its long-term safety, efficacy, and optimization of treatment regimens.
The potential risks, including transient side effects and the possibility of abuse and dependency, underscore the importance of careful clinical consideration. Despite these challenges, the promise of ketamine holds significant hope for transforming the therapeutic landscape of PTSD, potentially improving the lives of countless individuals affected by this debilitating disorder.
FAQS
Ketamine is most commonly administered as an intravenous infusion over a period of about 40 minutes. However, other routes such as intramuscular injection, oral, and intranasal are being studied.
As of now, insurance coverage varies. Some providers may cover it for depression, but coverage for PTSD is less common. It’s best to check with your specific provider.
While ketamine shows promise as a stand-alone treatment, it is often used in conjunction with other therapies, such as cognitive-behavioral therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR). This multi-modal approach can potentially provide a comprehensive treatment strategy for PTSD.