Understanding the ICD-10 Code for Hypertension
Hypertension, commonly known as high blood pressure, is a common medical condition that affects millions of people worldwide. It is characterized by a steady rise in blood pressure levels and poses a significant health risk if left unchecked. An accurate diagnosis is critical to the effective management and treatment of this condition.
In the medical community, the International Classification of Diseases, 10th Revision (ICD-10) is the accepted coding system used for diagnostic purposes. In this article, we will take an in-depth look at hypertension and reveal the specific ICD-10 code assigned to its diagnosis, shedding light on its importance in health care.
Understanding Hypertension
Hypertension occurs when the force of blood pressure on the walls of the arteries is consistently too high. This disease is often called the “silent killer” because it is asymptomatic, so people need to have their blood pressure checked regularly. Factors contributing to it include lifestyle, genetic predisposition, age, and underlying diseases such as obesity, diabetes, and kidney disease.
Hypertension is a chronic disease characterized by elevated blood pressure levels. It is the force with which blood presses against the walls of arteries as the heart pumps it throughout the body. It is measured in millimeters of mercury (mmHg) and is recorded as two values: systolic pressure and diastolic pressure. Systolic pressure represents the force when the heart is contracting and diastolic pressure represents the force when the heart is at rest between beats.
Normal blood pressure is usually considered to be 120/80 mmHg. However, if it is consistently above 130/80 mmHg, a diagnosis is made. Hypertension is a serious health problem because it puts extra strain on blood vessels and vital organs, potentially leading to various complications and diseases.
There are two main types of hypertension:
- Essential (primary): This is the most common form, accounting for approximately 90-95% of cases. It has no established cause and usually develops over time due to a combination of genetic and environmental factors. Risk factors include age, family history, obesity, sedentary lifestyle, excessive salt intake, alcohol consumption, and stress;
- Secondary: Secondary one is caused by an underlying disease or medication. It accounts for about 5-10% of cases. Various medical conditions can contribute to secondary hypertension, including kidney disease, endocrine disorders (such as adrenal or thyroid disease), certain medications (such as nonsteroidal anti-inflammatory drugs or birth control pills), and arterial narrowing (renal artery stenosis).
Hypertension is often called the “silent killer” because, in its early stages, it usually causes no noticeable symptoms. However, if left untreated or unchecked, it can lead to serious complications such as heart disease, stroke, kidney problems, vision loss, and blood vessels damage.
Diagnosis of hypertension involves regular blood pressure measurements taken repeatedly. The diagnosis is usually made if readings are consistently above the threshold. In addition, medical professionals may perform additional tests to identify underlying causes or assess organ damage.
The Main Causes of Hypertension
Hypertension, or high blood pressure, can be influenced by a combination of genetic factors, lifestyle, and environment. Although the exact cause of essential one (the most common type) is often unknown, several key factors contribute to the development of this condition.
Here are some of the main causes of hypertension:
- Family history: Hypertension is usually inherited, indicating a genetic predisposition to the disease. If your parents or close relatives have hypertension, you may have an increased risk of developing it;
- Age: Blood pressure tends to increase with age. This may be due to changes in the elasticity of blood vessels and an increase in the amount of plaque in the arteries.
Also, improper: Lifestyle can greatly contribute to the development of hypertension. These can include:
- Improper diet: A diet high in sodium (salt) and saturated fats can increase blood pressure. Also, inadequate intake of fruits, vegetables, and whole grains, as well as excessive consumption of processed foods can contribute to hypertension;
- Lack of physical activity: A sedentary lifestyle and lack of regular physical activity can increase the risk of developing this condition. Regular exercise helps maintain a healthy weight, improves cardiovascular health, and lowers blood pressure;
- Obesity: Being overweight or obese puts extra strain on the heart, which leads to an increased risk of developing hypertension. Being overweight can disrupt normal hormonal and metabolic processes that regulate blood pressure;
- Smoking: Smoking tobacco and secondhand smoke can temporarily increase blood pressure and damage blood vessels, increasing the risk of hypertension;
- Excessive alcohol consumption: Drinking large amounts of alcohol on a regular basis can increase blood pressure. It is recommended to limit alcohol consumption to moderate levels (up to one drink per day for women and two drinks per day for men);
- Stress: Chronic stress and elevated levels of stress hormones such as cortisol can contribute to high blood pressure.
Certain medical conditions can contribute to the development of hypertension. These include:
- Kidney disease: Kidney problems can upset the balance of fluids and electrolytes in the body, leading to high blood pressure;
- Endocrine disorders: Hormonal imbalances, such as an overactive thyroid gland (hyperthyroidism) or adrenal disease (such as Cushing’s syndrome), can contribute to hypertension;
- Sleep apnea: Sleep apnea, a disorder characterized by intermittent breathing during sleep, has been linked to hypertension. Repeated pauses in breathing can cause temporary spikes in blood pressure;
- Diabetes: People with diabetes are at higher risk of developing hypertension. Both diseases share common risk factors and can contribute to cardiovascular complications.
It is important to note that hypertension is a complex disease, and many factors can interact to raise blood pressure. Although some risk factors cannot be changed (such as age and family history), living a healthy lifestyle, managing stress, and seeing a doctor can help effectively prevent or manage it. Regular blood pressure checks and proactive health management are key to maintaining optimal blood pressure levels and reducing the risk of hypertension-related complications.
Management and Treatment of Hypertension
Management and treatment of hypertension usually include lifestyle changes and, if necessary, medication. Lifestyle changes may include following a healthy diet (low in sodium and rich in fruits, vegetables, and whole grains), exercising regularly, maintaining a healthy weight, limiting alcohol consumption, and managing stress levels. In some cases, healthcare providers may prescribe antihypertensive medications to lower blood pressure and reduce the risk of complications.
Regular control and treatment of hypertension are necessary to prevent long-term complications. Individuals diagnosed with it should work closely with their physicians to develop an individualized treatment plan and make necessary lifestyle adjustments to maintain optimal blood pressure levels.

ICD-10: The Standard Diagnostic Coding System
The International Classification of Diseases, 10th revision (ICD-10) is a comprehensive and standardized coding system used by health professionals around the world to classify and code diagnoses, symptoms, and medical procedures. This system provides consistent communication, efficient data collection, and streamlined healthcare practices.
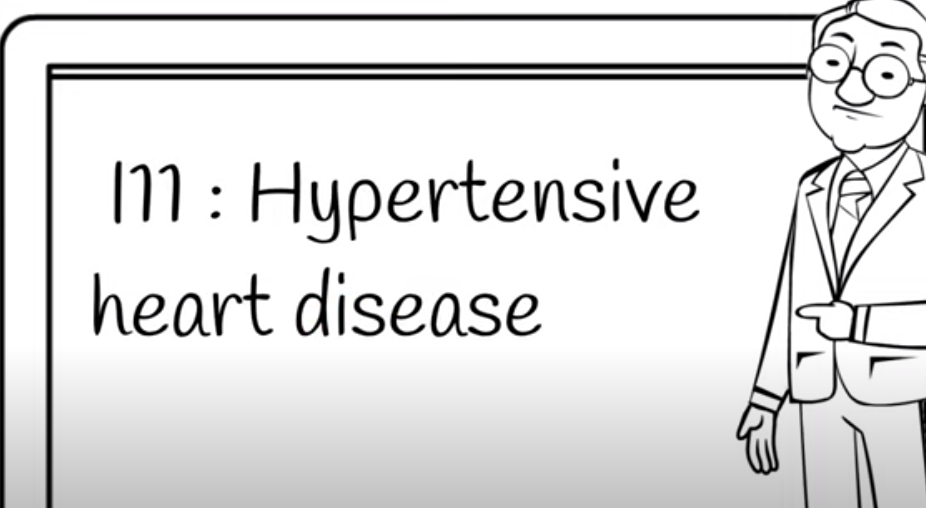
ICD-10 Code for Hypertension
In the ICD-10 system, hypertension is categorized as a Disease of the Circulatory System and is assigned a range of I10-I16 codes. Specifically, the I10 code is used to refer to essential (primary) hypertension, which means high blood pressure without any identifiable cause.
However, it can also have secondary causes. These include conditions such as kidney disease, endocrine disorders, and taking certain medications. In such cases, additional codes from the I15 category are used to clarify the underlying cause. For example, I15.0 indicates renovascular hypertension, and I15.1 indicates hypertensive heart disease with heart failure.
The Significance of Accurate Coding
Assigning the correct ICD-10 hypertension code is critical for several reasons. First, accurate coding allows health professionals to track the prevalence and incidence of hypertension, which facilitates public health research and policymaking. Second, it facilitates effective communication between healthcare providers, insurance companies, and government agencies, simplifying healthcare billing and reimbursement processes.
Moreover, accurate coding for hypertension ensures proper documentation of the disease in the medical history, allowing for better coordination of care and monitoring of treatment outcomes. In addition, accurate coding helps identify comorbidities and complications associated with hypertension, allowing for comprehensive management and prevention of related health problems.
Conclusion
Hypertension is a common disease that requires careful diagnosis and treatment. The ICD-10 coding system plays a critical role in accurately documenting and communicating hypertension diagnoses, assisting public health efforts, reimbursement processes, and patient care coordination. Using the specific ICD-10 codes assigned to hypertension, healthcare providers can provide effective treatment, monitoring, and prevention of this silent but potentially dangerous disease.