Understanding the Stages of Hypertension
Hypertension, or high blood pressure, is a ubiquitous yet largely unnoticed condition affecting millions worldwide. A nuanced understanding of its stages and practical management tips can help prevent severe complications. This article delves deeper into these aspects while addressing commonly asked questions about hypertension.
Defining Blood Pressure
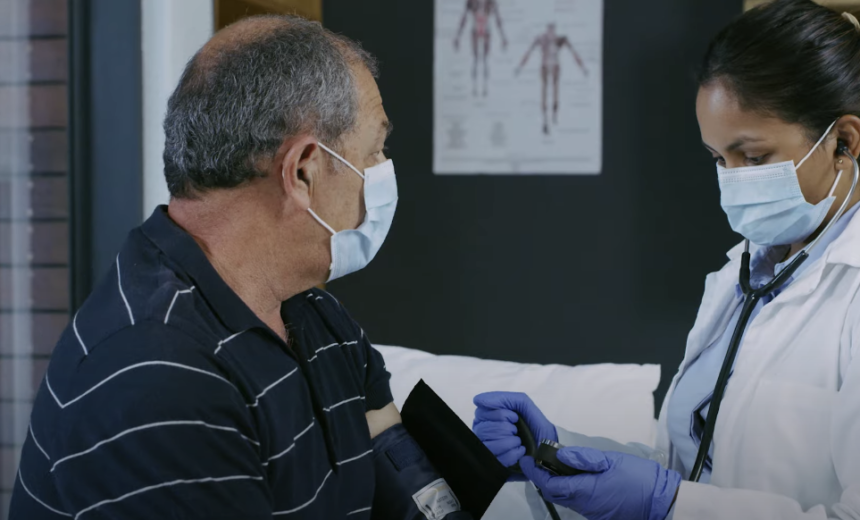
Blood pressure is the force exerted by circulating blood against the walls of the blood vessels. Measured in millimeters of mercury (mm Hg), it is presented as two values: systolic over diastolic. The systolic pressure indicates the force as the heart contracts and pumps blood, whereas the diastolic pressure signifies the force when the heart is at rest between beats.
Stages of Hypertension
Hypertension, or high blood pressure, is categorized into four stages based on systolic and diastolic blood pressure values. The stages help determine the severity of hypertension and guide treatment strategies. Let’s explore each stage in detail.
- Normal: Blood pressure is considered normal if the systolic reading is less than 120 mm Hg and the diastolic reading is less than 80 mm Hg. Individuals within this range are generally not at immediate risk, but it is still important to maintain a healthy lifestyle to prevent the progression towards hypertension. Even people with readings in the higher end of the normal range, ranging from 115/75 mm Hg to 120/80 mm Hg, should adopt healthy lifestyle changes to minimize the risk of developing hypertension;
- Elevated: The elevated stage serves as a preliminary warning sign that the blood pressure is higher than normal and indicates a potential progression towards hypertension. In this stage, the systolic blood pressure ranges from 120-129 mm Hg, while the diastolic reading remains below 80 mm Hg. Lifestyle modifications are particularly important at this stage to prevent the development of hypertension. These may include dietary changes, regular exercise, stress reduction techniques, and weight management;
- Stage 1 Hypertension: Stage 1 hypertension is diagnosed when blood pressure readings consistently fall within the range of 130-139 mm Hg systolic or 80-89 mm Hg diastolic. At this stage, physicians often recommend lifestyle changes as the first line of treatment. Lifestyle modifications may include adopting a low-sodium diet, increasing physical activity, limiting alcohol consumption, quitting smoking, and managing stress. In addition, physicians may consider prescribing blood pressure medication in certain cases, depending on the individual’s risk factors and overall health;
- Stage 2 Hypertension: Stage 2 hypertension is characterized by blood pressure readings consistently at 140/90 mm Hg or higher. This stage indicates a more severe form of hypertension and often requires a combination of lifestyle changes and medication to manage blood pressure effectively. Lifestyle modifications remain crucial, and physicians usually prescribe blood pressure-lowering medications to bring the readings within a healthier range. The specific medications and dosages may vary depending on individual circumstances, and regular monitoring is important to assess the effectiveness of the treatment.
Hypertension is classified into four stages: normal, elevated, stage 1 hypertension, and stage 2 hypertension. Each stage represents different blood pressure ranges and requires specific approaches to manage and control hypertension effectively. It is essential to work closely with healthcare professionals to develop a personalized treatment plan based on individual circumstances and risk factors.
Stage Systolic mm Hg Diastolic mm Hg Normal <120 <80 Elevated 120-129 <80 Stage 1 Hypertension 130-139 80-89 Stage 2 Hypertension ≥140 ≥90
Causes and Risk Factors of Hypertension
Understanding the root causes and risk factors associated with hypertension can provide valuable insights into preventive measures and management techniques. By analyzing these variables, one can take decisive action to mitigate the risk of hypertension.
Hypertension can be broadly categorized into two types: primary (or essential) and secondary.
- Primary Hypertension: This form of hypertension develops gradually over time with no identifiable cause. A combination of factors, such as genetic predisposition and environmental influences, plays a role in the onset of primary hypertension;
- Secondary Hypertension: This type tends to occur suddenly and causes higher blood pressure than primary hypertension. It is often the result of an underlying health condition such as kidney disease, hormonal disorders, or as a side effect of certain medications.
Having discussed these types, let’s delve deeper into the specific causes and risk factors associated with hypertension.
Family history is a significant risk factor for hypertension. If one or both of your parents had high blood pressure, your risk of developing the condition is higher. This influence is due to both genetic factors and shared environmental factors within families.
Age and Gender
Age is a considerable factor in the development of hypertension. Men are generally at a higher risk of developing hypertension from their mid-20s to mid-50s. After menopause, women’s risk surpasses men’s, highlighting the role of hormonal changes in blood pressure regulation.
Diet and Nutrition
Diet plays a critical role in blood pressure regulation. Diets high in salt, fat, and cholesterol, combined with low fruit and vegetable intake, can increase the risk of developing hypertension. The following dietary components contribute to high blood pressure:
- High Sodium Intake: Consuming too much sodium disrupts the natural balance, causing the body to retain fluid, which increases blood pressure;
- Low Potassium Intake: Potassium helps balance the amount of sodium in your cells. Insufficient potassium intake can lead to an accumulation of sodium in your blood;
- High Calorie Intake: Consuming excess calories can lead to weight gain, a primary risk factor for hypertension.
Sedentary Lifestyle and Physical Inactivity
Physical inactivity and a sedentary lifestyle contribute significantly to the development of hypertension. Regular exercise makes your heart stronger, and a stronger heart can pump more blood with less effort, thereby decreasing the force on your arteries and reducing your blood pressure. On the contrary, lack of physical activity leads to higher heart rates, causing your heart to work harder with each contraction, leading to hypertension over time.
Alcohol and Tobacco Use
Alcohol and tobacco use significantly contribute to the risk of developing hypertension.
- Alcohol: Consuming alcohol in moderate to high quantities can raise blood pressure to unhealthy levels;
- Tobacco: Tobacco products, including smoking and chewing tobacco, can raise your blood pressure. The chemicals in tobacco can damage the lining of your artery walls, causing your arteries to narrow and your blood pressure to increase.
Obesity
Weight gain is a crucial factor leading to hypertension. The more you weigh, the more blood you need to supply oxygen and nutrients to your tissues. As the volume of blood circulated through your blood vessels increases, so does the force on your artery walls, leading to higher blood pressure.
Psychological Factors
Stress can make a significant contribution to high blood pressure. When you’re stressed, your body produces a surge of hormones that temporarily increase your blood pressure by causing your heart to beat faster and your blood vessels to narrow.
Existing Health Conditions
Certain chronic conditions can increase your risk of developing hypertension. These include:
- Diabetes: Hypertension is twice as likely to occur in individuals with diabetes. This combination increases the risk of developing cardiovascular diseases;
- Kidney Disease: Hypertension can occur as a result of kidney disease. In return, high blood pressure can exacerbate kidney disease, leading to a vicious cycle;
- Sleep Apnea: Pauses in breathing during sleep lead to low oxygen levels in your blood, which can increase blood pressure.
Medications
Certain medications, including birth control pills, cold remedies, decongestants, over-the-counter pain relievers, and some prescription drugs, can cause blood pressure to rise.
In summary, a variety of factors contribute to the risk of developing hypertension. Some, like age and family history, are out of our control, while others, such as diet, physical activity, and substance use, can be modified to lower risk. Understanding these factors can guide interventions to prevent and manage hypertension effectively. It’s crucial to remember that regular monitoring of blood pressure is essential, irrespective of the presence of risk factors, as hypertension often has no noticeable symptoms until significant damage has occurred.
Managing Hypertension: Comprehensive Tips and Guides

Management of hypertension is multifaceted, involving lifestyle modifications and potential medical treatments. Here are detailed tips:
Title Description Healthy Eating The DASH (Dietary Approaches to Stop Hypertension) diet is often recommended. It focuses on fruits, vegetables, whole grains, lean proteins, and low-fat dairy, while limiting foods high in saturated fats and cholesterol. It involves increasing daily servings of vegetables and fruits, opting for whole grains, and using lean proteins such as poultry, fish, and legumes. Physical Activity Regular physical activity for at least 30 minutes most days of the week is beneficial. Physical activity can be moderate, like brisk walking, swimming, or mowing the lawn, or vigorous, like running, hill climbing, or sports like basketball and soccer. Limit Sodium Intake High sodium intake can raise blood pressure. Sodium intake should be less than 2,300 milligrams per day, but an even lower goal of 1,500 milligrams is ideal for most adults. Alcohol Moderation While moderate alcohol consumption may potentially lower blood pressure, excessive drinking can raise blood pressure and reduce the effectiveness of certain blood pressure medications. Quit Smoking Each cigarette raises blood pressure for several minutes after you finish. Quitting smoking helps your blood pressure return to normal. Weight Management Weight loss reduces the burden on your heart. Losing even a small amount of weight if you’re overweight can help lower your blood pressure.
Indications for Different Stages
Healthcare providers employ a comprehensive approach to determine the appropriate treatment plan for each stage of hypertension. The indications for different stages involve a combination of lifestyle modifications, medication, and immediate medical intervention in certain cases. The following information outlines the specific indications for each stage:
- Normal Blood Pressure and Elevated Blood Pressure:
- Lifestyle Modifications: The primary approach for individuals with normal blood pressure or elevated blood pressure involves healthy lifestyle modifications to maintain optimal blood pressure levels and prevent the progression towards hypertension;
- Regular Monitoring: It is advised to regularly monitor blood pressure to ensure it remains within the normal range.
- Stage 1 Hypertension:
- Lifestyle Modifications: In addition to healthy lifestyle changes, individuals with stage 1 hypertension may require medical treatment;
- Risk Factors: Individuals with heart disease or risk factors such as diabetes or chronic kidney disease may be more likely to require medical intervention.
- Stage 2 Hypertension:
- Lifestyle Modifications: Lifestyle changes continue to be crucial in stage 2 hypertension;
- Medication: The combination of lifestyle modifications and antihypertensive medications becomes crucial in this stage. Multiple medications may be necessary to effectively control blood pressure.
- Hypertensive Crisis:
- Immediate Medical Intervention: A hypertensive crisis occurs when blood pressure exceeds 180/120 mm Hg. In this situation, immediate medical intervention is necessary;
- Life-threatening Conditions: If left untreated, a hypertensive crisis can lead to life-threatening conditions such as stroke or heart attack.
While lifestyle modifications are important for all stages of hypertension, the need for medical treatment and the intensity of medication may increase as the stage progresses. In cases of a hypertensive crisis, immediate medical attention is vital to prevent severe complications. Regular monitoring of blood pressure is advised to ensure timely intervention and effective management of hypertension.
Conclusion
Understanding and managing hypertension is an integral aspect of overall health. The different stages of hypertension, ranging from normal to stage 2, highlight the progression of the disease and serve as an important guide for intervention. Each stage necessitates a specific approach, primarily involving lifestyle changes and, in more severe stages, medication. Knowledge about hypertension and proactive health measures can lead to better blood pressure control, mitigating the risk of life-threatening complications. Therefore, comprehensive understanding, regular monitoring, and optimal management of hypertension should be the priority for everyone striving for a healthier life.
FAQS
Hypertension is usually a chronic condition that can be effectively managed but not outrightly cured. With appropriate lifestyle modifications and medication, individuals can lead a healthy life.
Often known as the “silent killer,” hypertension typically doesn’t present noticeable symptoms until severe health problems arise. Rarely, some people may experience headaches, shortness of breath, or nosebleeds, but these are not specific to hypertension.
Lifestyle changes are the cornerstone of hypertension management and can significantly reduce the risk. However, for those in higher stages of hypertension, medication is often required alongside lifestyle changes.
Uncontrolled hypertension can lead to serious complications, including heart attack, stroke, heart failure, kidney disease, vision loss, and metabolic syndrome. These risks underscore the importance of maintaining optimal blood pressure.