Unveiling Ketamine Infusion Therapy: A Breakthrough
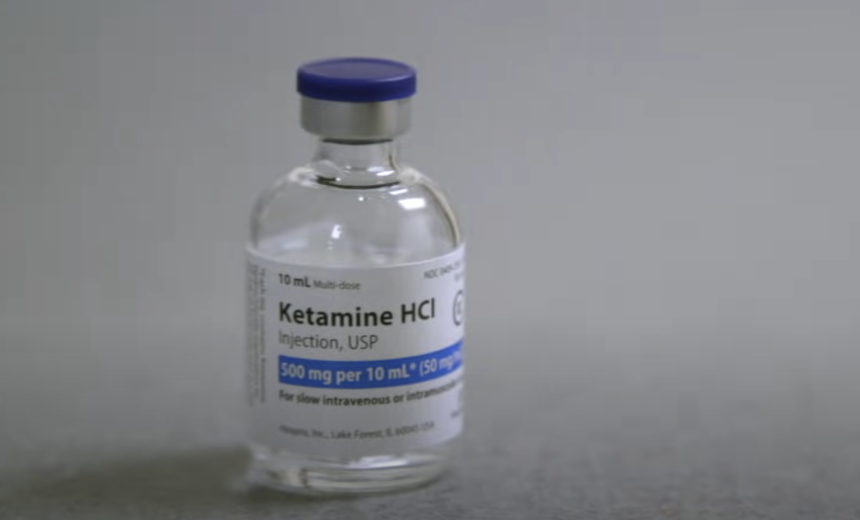
Ketamine, originally developed and approved by the FDA as a surgical anesthetic, has made a remarkable entry into the realm of mental healthcare through a groundbreaking approach called ketamine infusion therapy. This innovative method entails the administration of the drug intravenously, ensuring a consistent and controlled dosage.
Grasping the Composition of Ketamine
To truly comprehend the potential of ketamine infusion therapy, it is vital to grasp the chemical composition of ketamine. Ketamine falls under the category of dissociative anesthetics, which also encompasses substances like phencyclidine (PCP) and dextromethorphan (DXM). Its molecular structure can be represented as C13H16ClNO, and it possesses two optical isomers: S(+) ketamine and R(-) ketamine. These isomers contribute differently to the anesthetic and analgesic effects of ketamine.
Uses of Ketamine Infusion Therapy
Over the years, research has highlighted the potential role of ketamine in managing several medical conditions:
- Depression: This is particularly relevant for treatment-resistant depression, where patients haven’t responded to traditional antidepressants. Ketamine has been observed to provide rapid relief, sometimes within hours of administration, compared to weeks with other treatments;
- Post-traumatic Stress Disorder (PTSD): Early studies indicate that ketamine infusion may help manage symptoms of PTSD;
- Chronic Pain: Ketamine can help manage various chronic pain conditions such as fibromyalgia and CRPS, often when other treatments have been unsuccessful;
- Suicidal Ideation: Some studies have found that ketamine may have rapid anti-suicidal effects, which could be life-saving in acute situations;
- Anxiety and Obsessive-Compulsive Disorder (OCD): Preliminary research suggests ketamine could be beneficial in severe, treatment-resistant anxiety and OCD.
Mechanism of Action
Ketamine is a medication that has gained significant attention in recent years for its potential therapeutic effects in mental health conditions such as depression and post-traumatic stress disorder (PTSD). Although extensive research is underway, the precise mechanism through which ketamine functions is not fully understood. However, certain aspects of its action have been established.
Mechanism Description NMDA Receptor Blockade Ketamine primarily acts by blocking a specific receptor in the brain called the NMDA receptor. This receptor is involved in the transmission of signals between neurons and plays a crucial role in synaptic plasticity, learning, and memory formation. By blocking the NMDA receptor, ketamine disrupts the normal flow of information between neurons, leading to a disruption in neural circuits associated with mental health conditions. Glutamate Surge The blockade of NMDA receptors by ketamine leads to a surge in the levels of glutamate, which is another neurotransmitter in the brain. Glutamate is known to be involved in various brain functions, including neuronal communication and synaptic plasticity. The increase in glutamate levels triggered by ketamine is thought to be responsible for some of its therapeutic effects. BDNF Release The surge in glutamate resulting from ketamine’s action on NMDA receptors leads to the release of another substance called Brain-Derived Neurotrophic Factor (BDNF). BDNF is a protein that plays a crucial role in the growth, survival, and differentiation of neurons. It is involved in promoting the development and maintenance of neural connections, also known as synapses. The release of BDNF following ketamine administration stimulates the growth of new connections between brain cells, a process known as neuroplasticity. Enhanced Brain Function The increased release of BDNF and subsequent neuroplasticity induced by ketamine can potentially enhance overall brain function. By promoting the growth of new neural connections, ketamine may help to restore or strengthen disrupted neural circuits associated with mental health conditions. This enhancement of brain function could explain the observed rapid and robust antidepressant effects of ketamine. Alleviation of Symptoms The restoration of neural circuits and improved brain function resulting from ketamine’s mechanism of action may contribute to the alleviation of symptoms in mental health conditions such as depression and PTSD. By promoting synaptic plasticity and the formation of new connections, ketamine may help to mitigate the underlying neurological dysfunction that contributes to these disorders.
While the precise mechanism of action of ketamine is not yet fully understood, it is known to primarily act by blocking NMDA receptors, leading to a surge in glutamate and the subsequent release of BDNF. This release of BDNF stimulates neuroplasticity and the growth of new connections between brain cells, potentially enhancing overall brain function and alleviating the symptoms of mental health conditions. Further research is still ongoing to fully elucidate the complex mechanisms underlying ketamine’s therapeutic effects.
The Procedure of Ketamine Infusion Therapy
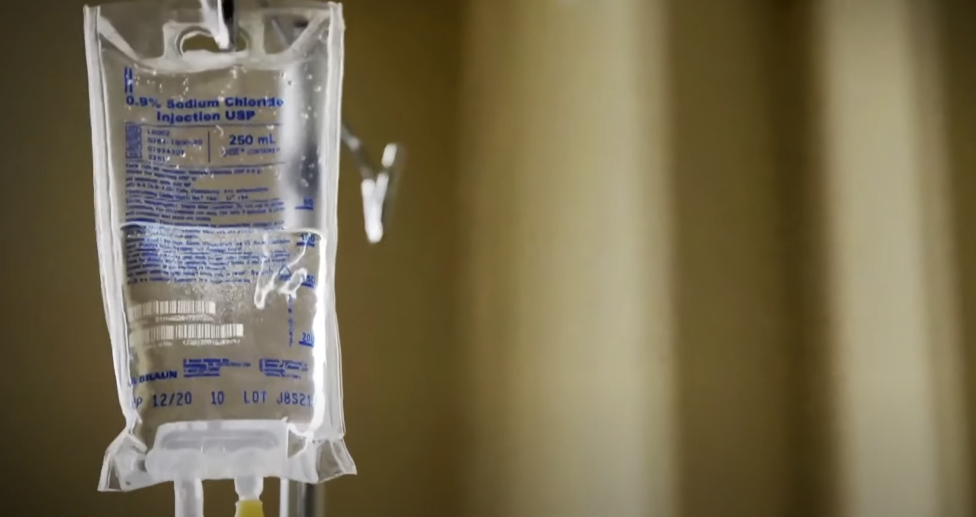
The ketamine infusion therapy procedure is a medical treatment that involves the administration of ketamine intravenously to patients. Here is a detailed breakdown of the steps involved in the procedure:
Procedure Description Patient Preparation The patient is seated comfortably in a reclining chair, providing a relaxed and supportive environment during the infusion. Vital signs, such as blood pressure, heart rate, and oxygen levels, are monitored to ensure patient safety and to establish baseline measurements. Intravenous Access A trained healthcare provider will identify a suitable vein, usually in the arm, for the administration of the ketamine infusion. The area is cleaned with an antiseptic solution, and a sterile needle is inserted into the vein to establish intravenous access. Ketamine Administration Once intravenous access is secured, the healthcare provider begins the infusion of ketamine. Ketamine is typically administered slowly and continuously over a specific period, usually lasting between 40 to 60 minutes. The exact dosage and infusion rate are determined based on the patient’s individual needs and response to treatment. Monitoring and Support Throughout the infusion, the patient’s vital signs and level of consciousness are closely monitored by the healthcare provider. Adequate monitoring ensures patient safety and allows for prompt intervention if any adverse effects or complications arise. The healthcare provider remains present during the entire infusion to provide support, address any concerns, and ensure a smooth experience for the patient. Post-Infusion Observation After the completion of the ketamine infusion, the patient is observed for a period of time to ensure a safe recovery. The healthcare provider continues to monitor the patient’s vital signs and assess their overall well-being. Depending on the specific protocol and individual patient factors, the observation period may vary, typically ranging from 30 minutes to a few hours.
It’s important to note that the specific details of the ketamine infusion procedure may vary depending on the healthcare provider, clinical setting, and individual patient needs. Prior to undergoing ketamine infusion therapy, patients should consult with their healthcare provider to understand the specific protocol, potential risks, and expected outcomes associated with the treatment.
Administration and Dosage

The administration and dosage of ketamine in infusion therapy require careful consideration to ensure both effective treatment and minimal side effects. Here are the key details regarding the administration and dosage of ketamine in this context:
Detail Description Dosage Range The dosage of ketamine used in infusion therapy is significantly lower than the doses used in anesthesia. This lower dosage allows for a more precise management of its therapeutic effects while reducing the likelihood of adverse reactions. Generally, the dosage of ketamine in infusion therapy ranges from 0.5 to 1.0 mg/kg of body weight. Infusion Duration Ketamine is typically administered over a specific period, usually lasting between 40 to 60 minutes. This slow and continuous infusion allows for a gradual onset of the therapeutic effects while ensuring patient safety and comfort. The exact duration of the infusion may be adjusted based on individual patient factors and the specific treatment protocol. Individualized Treatment The dosage and length of the infusion are individualized for each patient, considering various factors such as diagnosis, severity of symptoms, body weight, and overall health status. The healthcare provider will assess these factors to determine the optimal dosage and duration that will yield the desired therapeutic effects. Optimal Results By individualizing the treatment protocol, healthcare providers aim to achieve the best possible outcomes for each patient. The goal is to strike a balance between effectively managing the patient’s symptoms and minimizing any potential side effects associated with ketamine administration. Regular monitoring and evaluation of the patient’s response to treatment help guide adjustments in dosage and infusion duration if needed.
It is crucial to highlight that the specifics of the dosage and infusion duration may vary based on the healthcare provider’s expertise, the patient’s unique characteristics, and the particular treatment facility’s protocols. Patients should consult with their healthcare provider to understand the recommended dosage, infusion duration, and expected outcomes specific to their individual circumstances.
Potential Side Effects
Despite its potential benefits, ketamine infusion therapy may cause side effects. However, these are generally mild and transient. These can include:
- Psychological Effects: Some patients may experience hallucinations, panic attacks, or flashbacks to past traumas;
- Physiological Effects: Patients may also experience increased heart rate and blood pressure, nausea, dizziness, and in rare cases, severe abdominal pain;
- Post-infusion Effects: Patients may feel fatigued or experience coordination problems for a few hours post-infusion.
Most side effects typically resolve shortly after the infusion is complete, and patients are carefully monitored throughout the process to manage any potential adverse effects.
Contraindications and Precautions
Ketamine infusion therapy is considered safe for most patients, but there are certain medical conditions that may contraindicate its use or require special precautions. Here are the details regarding contraindications and precautions associated with ketamine infusion therapy:
Contraindications
- Uncontrolled Hypertension: Patients with uncontrolled high blood pressure may be contraindicated for ketamine infusion therapy due to the potential cardiovascular effects of the medication;
- Unstable Heart Disease: Individuals with unstable heart disease, such as recent heart attack or severe congestive heart failure, may be at higher risk of adverse cardiac events during ketamine infusion therapy;
- Active Substance Misuse: Patients who currently misuse substances, including drugs and alcohol, may not be suitable candidates for ketamine infusion therapy due to the potential for interactions and increased risks;
- Liver Disease: Severe liver disease, such as advanced cirrhosis or liver failure, may impair the metabolism and clearance of ketamine, leading to an increased risk of side effects;
- History of Psychotic Disorders: Individuals with a history of psychotic disorders, such as schizophrenia or bipolar disorder with active psychosis, may be at higher risk of exacerbation of their symptoms during ketamine infusion therapy.
Precautions
While not absolute contraindications, the following conditions require special precautions and careful consideration before initiating ketamine infusion therapy:
- History of Substance Misuse: Patients with a history of substance misuse should be closely monitored and evaluated for their readiness and suitability for ketamine infusion therapy;
- Cardiovascular Conditions: Individuals with cardiovascular conditions, such as hypertension or stable heart disease, may require careful monitoring of their blood pressure and heart function during the infusion;
- Respiratory Conditions: Patients with respiratory disorders, such as asthma or chronic obstructive pulmonary disease (COPD), may need additional monitoring due to the potential for ketamine to cause respiratory depression;
- Pregnancy and Breastfeeding: The safety of ketamine infusion therapy during pregnancy and breastfeeding has not been extensively studied, and thus caution should be exercised in these situations.
It is crucial for healthcare providers to thoroughly assess a patient’s medical history, including any contraindications or precautions, before initiating ketamine infusion therapy. Open communication between the healthcare provider and the patient is essential to ensure the appropriateness and safety of the treatment.
Please note that this list is not exhaustive, and healthcare providers may consider other individual factors when determining the suitability of ketamine infusion therapy for a particular patient.
The Future of Ketamine Infusion Therapy
Research on ketamine infusion therapy is still in its early stages, and there’s much we don’t yet know. However, early findings are promising, and ongoing studies continue to explore its potential applications in various areas of mental health.
Potential Applications of Ketamine Infusion Therapy
| Disorder | Description |
|---|---|
| Treatment-Resistant Depression | Ketamine infusion therapy has shown promising results in the treatment of individuals with treatment-resistant depression. Traditional antidepressant medications may take several weeks to produce noticeable effects, but ketamine has been observed to provide rapid relief within hours or days. Ongoing research aims to further understand the mechanisms of ketamine’s antidepressant effects and refine treatment protocols. |
| Post-Traumatic Stress Disorder (PTSD) | Early studies have suggested that ketamine infusion therapy may have potential in treating symptoms of PTSD. It has been hypothesized that ketamine’s ability to modulate glutamate receptors in the brain could help alleviate the intrusive thoughts and hyperarousal associated with PTSD. Further research is needed to validate these initial findings and determine optimal dosage and treatment duration. |
| Anxiety Disorders | Anxiety disorders, including generalized anxiety disorder (GAD) and social anxiety disorder (SAD), can be debilitating for individuals. Preliminary evidence suggests that ketamine infusion therapy may offer relief for these conditions as well. Ongoing research aims to explore the effectiveness and long-term outcomes of ketamine treatment for anxiety disorders. |
| Suicidal Ideation and Self-Harm | One of the most significant discoveries in recent years is ketamine’s potential to rapidly reduce suicidal ideation and self-harm behaviors in individuals at risk. Studies have shown that ketamine infusion therapy can lead to a significant reduction in suicidal thoughts within hours or days. This finding has sparked hope for the development of effective interventions for individuals experiencing acute suicidality. |
| Substance Use Disorders | Research is underway to investigate the potential of ketamine infusion therapy in the treatment of substance use disorders, such as alcohol and opioid dependence. Preliminary studies suggest that ketamine may help reduce cravings and withdrawal symptoms, potentially aiding in the recovery process. Further investigation is necessary to establish the safety, efficacy, and long-term outcomes of ketamine treatment in this context. |
Challenges and Future Directions
While the early results of ketamine infusion therapy are promising, there are several challenges and areas for future exploration:
- Mechanisms of Action: The exact mechanisms through which ketamine exerts its therapeutic effects are not fully understood. Further research is needed to elucidate the neurobiological processes involved and identify specific molecular targets;
- Treatment Protocols: Standardized treatment protocols for ketamine infusion therapy have not yet been established. Determining optimal dosages, treatment durations, and frequency of sessions is crucial for maximizing therapeutic benefits while minimizing potential risks;
- Long-term Effects and Safety: Long-term effects and safety considerations of ketamine infusion therapy are still being investigated. Questions remain regarding potential cognitive and psychomotor impairments, the risk of abuse or addiction, and the sustainability of treatment effects over time;
- Accessibility and Affordability: Ketamine infusion therapy currently faces accessibility and affordability challenges. The therapy is often expensive, and access is limited to specialized clinics or research settings. Efforts to increase accessibility and reduce costs are necessary for widespread adoption and equitable availability.
Conclusion
Ketamine infusion therapy presents a significant advancement in the management of mental health and pain conditions. As research continues to evolve, it’s poised to revolutionize the way we understand and approach the treatment of these conditions. Despite this, it’s crucial for patients to have an open discussion with their healthcare providers to understand the benefits, potential risks, and overall suitability of this innovative treatment for their individual health needs.
FAQS
Unlike other depression treatments, ketamine infusion therapy works rapidly, often within hours, compared to weeks for other antidepressants. Also, it operates through a different mechanism, making it a valuable option for individuals not responding to traditional treatments.
Yes, in most cases, you can continue your existing mental health medications. However, this should be discussed with your healthcare provider.
The duration of the effects varies widely among individuals. Some may experience symptom relief for several weeks after a single infusion, while others may require regular infusions to maintain the effects.
No, only trained medical professionals in a controlled medical setting should administer ketamine infusion therapy.